Features
The Prospects for Creating Personal Decompression Plans
Why the Future of Dive Safety Hinges on Cracking the Code of Human Physiology
Limited technology, an absolute dearth of reproduceable data, and the need for a repeatable and modifiable algorithm are all that stand between you and a personalized decompression model for your next dive. If it sounds like a lot – it is.
The stark reality is that the best and brightest minds in hyperbarics have spent their careers making – sometimes huge and often fascinating – advances in research that not only cannot be applied to the real world, but cannot be correlated with any yet-identified physiologic or biologic metric. We have strong evidence that decompression sickness (DCS) is caused by intracorporeal bubble formation resulting from supersaturated dissolved gas, but recent data suggests that the quantity of those bubbles alone is not enough to predict whether someone will experience DCS symptoms1.
Knowing what most likely causes DCS is a weak enough base to build a decompression algorithm on but the issue is compounded on all fronts. Researchers have chased dozens of biometric markers in the hopes of correlating them with DCS symptoms, but none managed to do so in a reliable way (at least not yet). Measuring these markers is difficult in a lab and in most cases impossible to monitor during a dive, and current decompression algorithms are not designed to take any of these metrics into consideration.
Making the leap from the probabilistic decompression algorithms we currently use is going to require breakthroughs in decompression models, physiological monitoring tools and our understanding of the physiology of decompression.
Making the leap to a personalized decompression algorithm is going to require breakthroughs in decompression modeling, physiological monitoring tools, and our understanding of DCS. It’s a tall order by any measure but the potential for a single breakthrough to completely change our understanding of decompression modeling absolutely exists – and it’s what makes this research so exciting.

Dive deeper into what we know about personalized DCS modeling, what we need to know, and what research to keep an eye on:
Why Personalized Decompression Hasn’t Been Cracked – Yet.
The issues with decompression modeling begin at the most basic level, with our understanding of DCS. We think bubbles cause DCS symptoms, but there hasn’t yet been any solid data showing a correlation between bubble load or size and DCS. Complicating matters further there’s a whole slew of research indicating that it might not be the bubbles themselves causing injuries but the body’s response to those bubbles2. Without an understanding of the mechanism of injury behind DCS, even our best decompression algorithms become loose estimates of risk from decades old studies. Effectively, most of us are still diving an algorithm based on data derived from giving goats DCS more than a century ago – if the goats survived the dive, then you probably will too.
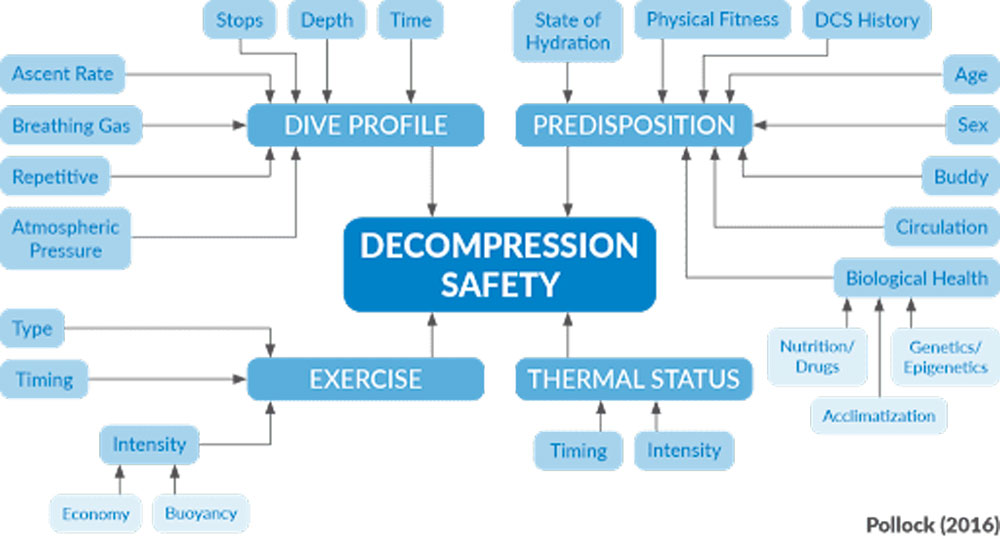
Current decompression algorithms are rudimentary at best but “staggeringly incapable of assessing a host of complex factors and timings that can influence gas uptake, elimination, and effective risk,” says decompression physiology expert Neal Pollock, Ph.D, adding that decompression algorithms are useful for a “first order approximation of risk – getting into the ballpark”. Beyond this point, Pollock advocates for divers to use algorithms as a base upon which to make conservative modifications based on experience and research, even though there will inevitably be a lot of supposition and guesswork.
The next hurdle for researchers is finding a metric to measure DCS risk, and then inventing the technology to assess it in real time. Personalizing decompression requires measuring something about a diver – whether that be temperature, epigenetic markers, or one of dozens of other possible physiological or biological markers. Fascinating to research but difficult to quantify, these represent the most interesting area of this conundrum for most divers.
Personalizing your decompression algorithm and reducing your risk of DCS in a meaningful way may not be possible by the time you hit the water next, but there’s a very real chance of one of these ongoing studies causing a complete evolution in the way we manage diver risk in the relatively near future.
Factors with a Future
Algorithms and new monitoring tools are fun to build but the truly thrilling part of this is the research into new DCS markers that could correlate with DCS risk – or even lead to a real understanding of the mechanism of DCS. There are too many of these to count, and it’s impossible to know which (if any) will ultimately provide insight into why we bubble the way we do, but the potential for breaththrough feels tantalizingly close in some areas. Here are two areas you should watch in the coming years:
Microparticles and Inflammatory Response
There’s a growing body of research suggesting that some of the harm caused by DCS is done not by mechanical damage from VGE formation during decompression, but by microparticles caused by bubble formation and the inflammatory responses to both the bubbles and the microparticles13,14. The proposed mechanisms for microparticle and inflammatory response to decompression and their contributions to DCS risk are somewhat convoluted and could be the subject of their own article, but an excellent summary can be found in Decompression Illness: A Comprehensive Overview, a 2024 summary by expert in the field Dr Simon Mitchell.
Microparticles and the inflammatory cytokines that these theories focus on can be measured – but only in a lab and not in real-time. More work needs to be done in this area to determine the relationship between oxidative stress, decompression and circulating microparticles before meaningful progress can be made but the interplay between the three and the data that does exist makes this a topic to pay particular attention to in the coming years.

Bubble Studies
Decades of suggestive (but not conclusive) research have indelibly linked bubbles and DCS, but a recent study from the NEDU and University of Auckland may have put the final nail in the coffin connecting VGE loads and DCS symptoms. Researchers took 151 divers and put them through 693 dives, performing bubble studies after each. The result was a uniquely large data set for this area of research, and one that strongly suggests that the variability of bubble quantity in the divers was great enough that not only can bubble counts not be used to evaluate decompression practices between divers, but that individual divers on identical dives will bubble at such a different rate that VGE grade may not have any meaningful correlation with DCS at all.
This throws a bit of a wrench in the status quo of diving research, but it’s not the end of bubble studies. DAN researchers have recently finished data collection on a 4 year project aimed at quantifying VGE load variability and looking at metrics like heart rate variability, cardiac output, blood pressure, saliva samples for inflammatory markers, and blood samples for microparticles. Data crunching has just begun, but short term analysis will be focusing on correlating DCS risk factors and bubble counts, and the research subject group has been maintained to facilitate follow-up studies.

Looking To the Future
Despite much of this research relying on still unproven mechanisms of DCS, and yet-undeveloped technology and biomarkers – there are a lot of reasons to be optimistic. Tempering that optimism with the knowledge that it may be years before the technology even exists to measure some of these theoretical markers in a meaningful way is needed, but it’s hard not to get excited about the sheer number of possibilities in this area.
Personalized decompression may not yet be a reality, but the hurdles to get there are identifiable and some brilliant researchers and divers are devoting their lives to making it possible. Interested in advancing the cause? You can learn about ongoing research projects and volunteer to help at https://www.daneurope.org/en/diving-medical-research
An extended version of the article was published in InDEPTH magazine.
Works Cited
- Doolette, D; Murphy, G (2023) Within-diver variability in venous gas emboli (VGE) following repeated dives.
- Mitchell, Simon J (2024) Decompression Illness: A comprehensive review. PMID: 38537300
Further reading
- Cialoni, D; Pieri, M; Balestra, C; Marroni, A (2017) Dive Risk Factors, Gas Bubble Formation, and Decompression Illness in Recreational SCUBA Diving: Analysis of DAN Europe DSL Data Base
About the author
Reilly Fogarty is a New England based rebreather instructor and USCG licensed captain. His professional background includes surgical and wilderness emergency medicine, Hyperbarics research and large-scale diving risk mitigation and first aid program design and management. He has previously worked on human trials in extreme exposure physiology for the Duke Center for Hyperbaric Medicine and Environmental Physiology and as the Risk Mitigation Team Lead for Divers Alert Network.

