Medical line
HRV and Decompression Induced Physiological Stress
Editor’s note: We present here a contributor’s analysis on a recent and vastly debated topic, shedding light on a study in which DAN Europe researchers are also involved. The article explores the intricate link between Heart Rate Variability (HRV) and decompression stress.
There’s nothing divers love more than finding a way to shave five minutes off their decompression, whether the justification is a particularly tasty surface snack waiting on the surface or some serious research data.
Thanks to recent work by a team of Brazilian and Italian researchers, and a quickly expanding understanding of decompression illness, you may soon be able to change the way you plan your decompression dives in a serious way. Working to develop a tool to better quantify decompression stress in divers, the team managed to correlate a metric historically used in cardiovascular medicine with known markers of decompression stress. Using this metric, the approach has been to look at decompression illness not as a disease caused by a few rogue bubbles, but as a multifaceted illness triggered by the factors we’re familiar with and driven by the physiological responses to those triggers.

It’s not that decompression illness isn’t about bubbles anymore, but that it’s not just about bubbles. In the past decade a host of new research has illustrated a model for decompression sickness that relies on a constantly growing number of physiological responses and increasingly complex biochemical mechanisms. The catalyst for this shift in understanding has primarily been the involvement of endothelial dysfunction research in decompression sickness. Signalling and response processes from endothelial cells have been linked to numerous disease processes and interest in these processes and the contributions of inflammatory processes to known diseases have exploded. Endothelial dysfunction is complex and our understanding of it is still evolving. But what’s important to understand is that modern research has shown that even diseases that we thought were well understood may not be the product of a single offensive agent but a combination of a trigger and the body’s own responses – in some cases the disease may be entirely caused by the body’s own response to that trigger.
Unfortunately, this means that we can no longer think of decompression illness as a simple disease caused by bubbles in the bloodstream. In reality it’s been shown that venous gas emboli (actual bubbles in the blood) are a poor indicator of DCS, and hugely variable between divers. Instead endothelial dysfunction has been correlated with hyperbaric exposure, and with it researchers have had to take a deep dive into inflammatory processes and what lies between the actual dives we do, and the decompression sickness that may follow.
The Role of Heart Rate Variability (HRV)
Enter heart rate variability (HRV) – used as a potential shorthand for a measure of specific inflammatory responses, it’s been correlated with a range of conditions from diabetes to cardiovascular disease, and shown to change with diving. That’s where this most recent study enters the fray. It’s been shown that microparticles in the blood have been correlated to inflammation, HRV has been shown to change with diving and correlated with inflammation, and microparticles have been shown to increase with exposure to inert hyperbaric gases, so it’s possible that HRV could be used as a convenient tool to measure the inflammatory responses in divers and potentially estimate risk of decompression illness. If this sounds ambitious, that’s because it is, but if the correlation between heart rate variability and decompression-induced physiological stress could be validated it would prove enormously powerful both as a tool for understanding how and why divers get injured, what the physiological responses to decompression stress are, and provide a method to estimate decompression risk in the field. We’re not there yet but this is an exciting first step, and the kind of thing that bubble nerds dream about.
The foundational research is a bit complex but the crux of this study is the idea that HRV can be correlated with inflammatory markers associated with decompression illness, and directly used as a measure of decompression illness risk. Specifically, the Brazilian and Italian researchers looked at markers taken from blood samples and ECG results to begin to correlate HRV with these inflammatory markers. Twenty-eight volunteers were each put through two separate dive profiles at one of three facilities where subjects used either closed circuit rebreathers, hyperbaric chamber supplied breathing gas or open-circuit Scuba equipment. The dive profiles all had the same total decompression time and gas supersaturation, though they varied in decompression stop depths in order to include some variation. Intervals between dives and data collection intervals were the same.
Researchers consolidated the data between the two profiles so they could be analyzed as a single data set. Pre- and post- dive ECG and blood samples were obtained with a 30 minute buffer before and after each dive, and a minimum of 48 hour interval was required between dives to prevent skewing of data due to lingering effects from prior exposure.
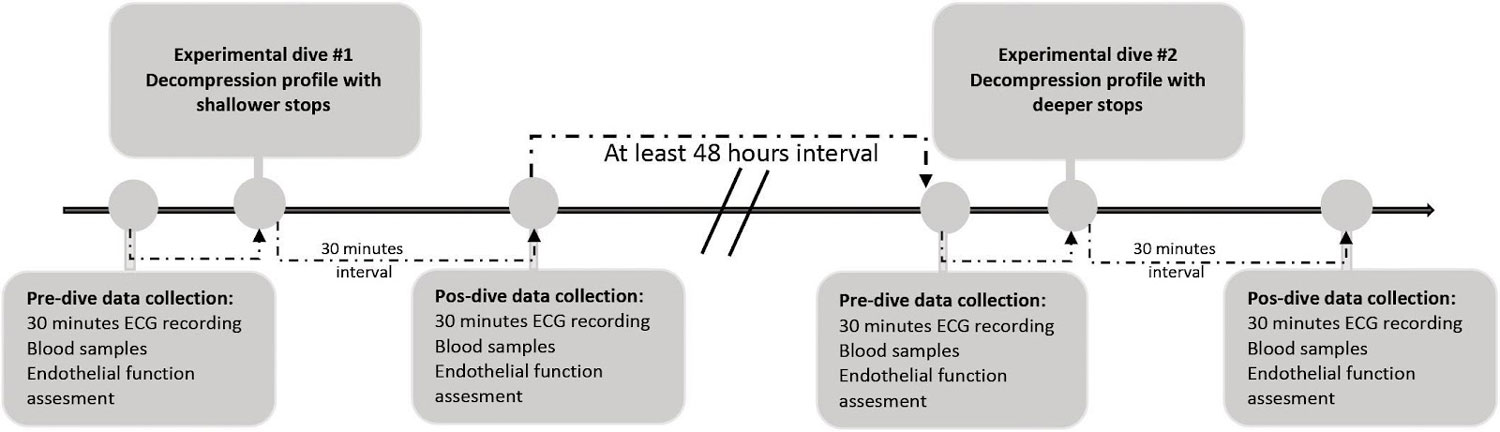
Image: Procedure flow chart – Association Between Heart Rate Variability and Decompression – Induced Physiological Stress
Significant accumulated results were analysed in a way best described by the authors themselves, then used to create a theoretical model to extrapolate the results taken from the relatively small sample group and model them on a dataset including approximately 1000 dives. There are a number of interesting avenues to pursue among the post-analysis data points but the focus on the relationship between HRV and the inflammatory markers showed a statistically significant change that could show serious promise.
The data can be intimidating but the key trends can be seen in the relationship between HF and SDNN, Annexin and MP, and the positive association between LF and CD66b+ and CD31+ MPs. For those lost in the wash of acronyms (see definitions below), all of that essentially means that multiple data correlations seem to converge in a way that provides statistically valid evidence for the researchers’ hypotheses.
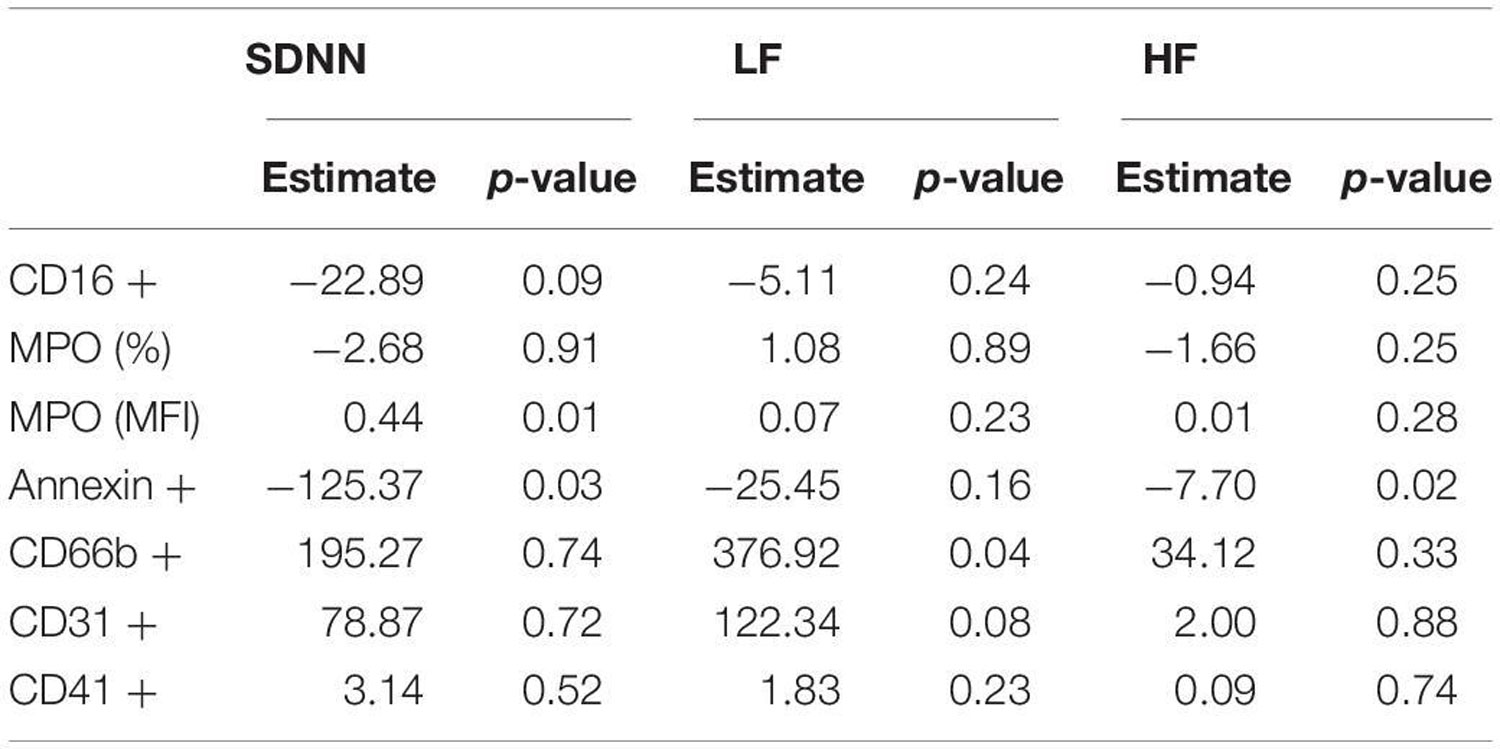 Post-modeling relationships between HRV indicators, MPO and MP – Association Between Heart Rate Variability and Decompression – Induced Physiological Stress
Post-modeling relationships between HRV indicators, MPO and MP – Association Between Heart Rate Variability and Decompression – Induced Physiological Stress
Note: LF and HF are low- and high- frequency band filters used during ECG studies – both represent different facets of electrocardiographic HRV analysis. The differences are not critical to the overall understanding of this study but more information is available for those interested.
In Conclusion
If all of this strikes you as a bit dense for a casual afternoon read, that’s because it is. The number of variables that affect inflammatory processes, decompression illness, and even day to day HRV data in the same subject are almost immeasurable, and accounting for as many as possible takes an enormous amount of foundational research and experimental planning. Understand the models enough to validate the research, then focus on the results – which in this case primarily seem to indicate a correlation between HRV after decompression, and the indicators of physiological inflammation and stress chosen by the investigators. This is by no means a reason to buy a heart rate monitor and cut your decompression as short as you can, but it is a promising result and an exciting potential for the future. It’s worth noting that data from animal models didn’t correspond to the human trials but didn’t provide anything to directly contradict the conclusions from the human studies. In addition, results may vary in cases of subjects experiencing decompression sickness, but the possibilities for future research are enormous.
If this relationship between HRV and decompression stress can be validated further it is possible that decompression models could be qualitatively validated by divers in real time, and a real understanding of the unknowns between tissue supersaturation and decompression illness could finally be possible. If this model is validated, we could be looking at fundamental changes in the way decompression is planned, and decompression illness is understood and treated.
With the ability of popular consumer technology to identify cardiac arrhythmias through a wrist watch, it’s not impossible that we could eventually see something like this HRV modelling incorporated in dive computers in the future. This isn’t something that should change the way you dive now, but this study and research into new models of multi-faceted understandings of decompression illness should absolutely excite you for the future.
Definitions
HF: High Frequency band of heart rate
LF: Low frequency band of heart rate
SDNN: Standard deviation of the (internet) IBI intervals measured in ms
Annexin: Annexin is a common name for a group of cellular proteins mostly found in animal, plant and fungi.
MP: Microparticles
MPO: Myeloperoxidase-positive microparticles
CD66b+: CD66b is an activation marker for human granulocytes; however, its biological functions are largely unknown in eosinophils.
CD31+: is known as platelet endothelial cell adhesion molecule
Works Cited:
- Brubakk, A. O., Duplancic, D., Valic, Z., Palada, I., Obad, A., Bakovic, D., et al. (2005). A single air dive reduces arterial endothelial function in man. J. Physiol. 566, 901–906. doi: 10.1113/jphysiol.089862
- Papadopoulou, V., Germonpré, P., Cosgrove, D., Eckersley, R. J., Dayton, P. A., Obeid, G., et al. (2018). Variability in circulating gas emboli after a same scuba diving exposure. Eur. J. Appl. Physiol. 118, 1255–1264. doi: 10.1007/s00421-018-3854-7
- Doolette, D. J. (2016). Venous gas emboli detected by two-dimensional echocardiography are an imperfect surrogate endpoint for decompression sickness. Diving Hyperb. Med. 46, 4–10.
- Cognasse, F., Hamzeh-Cognasse, H., Laradi, S., Chou, M.-L., Seghatchian, J., Burnouf, T., et al. (2015). The role of microparticles in inflammation and transfusion: a concise review. Transfus. Apher. Sci. 53, 159–167. doi: 10.1016/j.transci.2015.10.013
- Noh, Y., Posada-Quintero, H. F., Bai, Y., White, J., Florian, J. P., Brink, P. R., et al. (2018). Effect of shallow and deep SCUBA dives on heart rate variability. Front. Physiol. 9:110. doi: 10.3389/fphys.00110
- Appel, M. L., Berger, R. D., Saul, J. P., Smith, J. M., and Cohen, R. J. (1989). Beat to beat variability in cardiovascular variables: noise or music? J. Am. Coll. Cardiol. 14, 1139–1148. doi: 10.1016/0735-1097(89)90408-7
- von Känel, R., Nelesen, R. A., Mills, P. J., Ziegler, M. G., and Dimsdale, J. E. (2008). Relationship between heart rate variability, interleukin-6, and soluble tissue factor in healthy subjects. Bone 23, 1–7. doi: 10.1038/jid.2014.371
- Schirato SR, El-Dash I, El-Dash V, Bizzarro B, Marroni A, Pieri M, Cialoni D and Chaui-Berlinck JG (2020) Association Between Heart Rate Variability and Decompression-Induced Physiological Stress. Front. Physiol. 11:743. doi: 10.3389/fphys.2020.00743
About the author
Reilly Fogarty is a New England based rebreather instructor and USCG licensed captain. His professional background includes surgical and wilderness emergency medicine, Hyperbarics research and large-scale diving risk mitigation and first aid program design and management. He has previously worked on human trials in extreme exposure physiology for the Duke Center for Hyperbaric Medicine and Environmental Physiology and as the Risk Mitigation Team Lead for Divers Alert Network.

