All that tingles is not bends
Divers are taught to pay attention to any abnormal signs and symptoms after diving. They are instructed to consider them as being possible decompression illness (DCI) until proven otherwise. However, this attitude not only adds a certain amount of anxiety, but may also lead to an unhealthy level of attentiveness and concern about completely benign conditions that appear during or following diving activities.
Mild headaches, mild transient joint aches, skin irritations and even mild tingling or numbness may be attributed to DCI quite erroneously resulting in unnecessary medical evacuations, hospital admissions, recompression treatment and even the loss of diving fitness or a subsequent fear of diving. On the other hand we do not want to discourage divers from seeking assistance nor should they deny or overlook potentially serious manifestations of DCI. So there is a need to assist divers in better distinguishing between benign and serious conditions.
First of all, the risk can be reduced: Limiting the probability of developing decompression disorders by performing 5-S (i.e., Shorter, Shallower, Sensible with Safety Stops) dives will reduce the concern that minor symptoms may be bubble-related. It does not eliminate the risk, however, and we would like to caution divers not to fall into the “I-was-diving-within-the-tables-so-I-cannot-be-bent fallacy. As many as 50% of DCI cases in the DAN DCI database were diving within table or computer limits. However conservative diving does reduce the chances of developing serious DCI even if symptoms were to occur.
Another way to exclude an unnecessary over-diagnosis of DCI is to recognize certain common patterns of symptoms that are known to be due to causes other than DCI even though they may be associated with diving activities. For instance, in the previous edition of Alert Diver we addressed the various causes of diving-related headaches. So in this article we will be discussing paraesthesias (i.e., Greek for “partial excitement” or “feeling”) – which is an abnormal skin sensation usually described as burning, pins and needles or tingling.
Paresthesia and neuropraxia
Paraesthesia or tingling is the result of a partial interruption of sensory nerve conduction between the skin and the sensory cortex (i.e., the part of the brain responsible for making us aware of skin sensations).
Anaesthesia is the result of a complete interruption of impulses. In most cases, paraesthesia is a very temporary and benign condition. Often it is the result of direct pressure on a peripheral cutaneous nerve (i.e., skin nerve) due to a prolonged application of external pressure to the skin overlying a nerve. An example of this is the numbness that follows sitting in a fixed position for a period of time.
These mild crushing or stretching injuries to nerves are called neuropraxias. This means that the structure of the nerve is preserved but it ceases to transmit impulses for a period of time. In most cases reversal of symptoms follows pressure relief to the area almost immediately. However with long periods of pressure it may take several days and in rare cases even weeks for skin sensation to recover and for tingling to subside. This may happen when wearing tight-fitting or heavy gear such as a tight fitting wetsuit, weight belt or heavy BC-tank configuration for extended periods of time.
Because any interruption in nerve conduction between the skin and the brain can potentially cause these disturbances, it is important to determine the underlying cause. Short-term neuropraxia due to a tight-fitting wetsuit is much less significant than arterial gas embolism or decompression sickness. Yet both may cause numbness and tingling. Fortunately it is possible to make these distinctions fairly easily with a little bit of background knowledge. That is one of the objectives of this article – knowing when tingling is serious and when is it not.
The Brain, Spinal Cord and Nerves
Both paresthesia and anesthesia may be the result of damage to the brain, spinal cord or nerves. However, each of these latter injuries has a very specific distribution and it is possible therefore to make distinctions fairly easily.
The Brain
The brain contains several functional areas. The surface layer of the brain (also called the grey matter) is where we perform conscious thinking; where voluntary movements are initiated (called motor function); and the where the various physical sensations and the signals from our five special senses reach our consciousness (called sensory function). The picture below shows how the brain is divided into the coronal plane (A); followed by a coronal section of the brain (B); with a further illustration showing where the sensations from various body parts are recorded on surface of the brain (C).
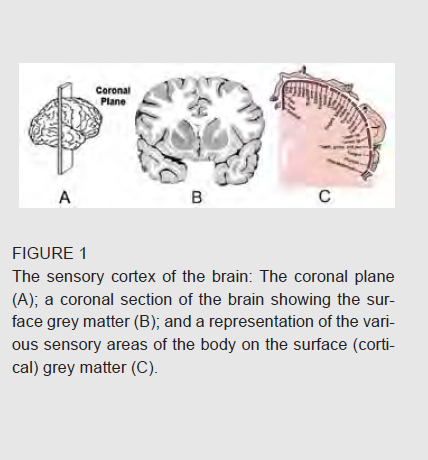

What should be obvious from this illustration is that a small injury to the cortex will result in a large area of skin numbness or tingling. Accordingly, cortical parasthesia – as this is called – usually affects an entire arm or leg. It is rare for both arms or both legs to be affected simultaneously, however. The typical impairment involves the left or the right side of the body respectively (i.e., hemi-paresthesia or hemi-anesthesia) and there is usually an associated weakness or paralysis of the affected area (i.e., hemiparesis).Therefore large areas of numbness – especially if a whole arm or leg is affected and there is associated weakness or paralysis – are very suspicious of brain involvement and require urgent medical attention.
Spinal cord
Like our brain, the spinal cord also contains areas responsible for relaying impulses for movement and sensation. There are also a large number of interconnecting filaments (axons) that run between the brain and the target organs or tissues. The spinal cord is arranged like a stack of cylindrical disks in the unborn embrio (Figure 2). Each disk has a segmental nerve supply and maintains this relationship as the embrio grows and changes shape
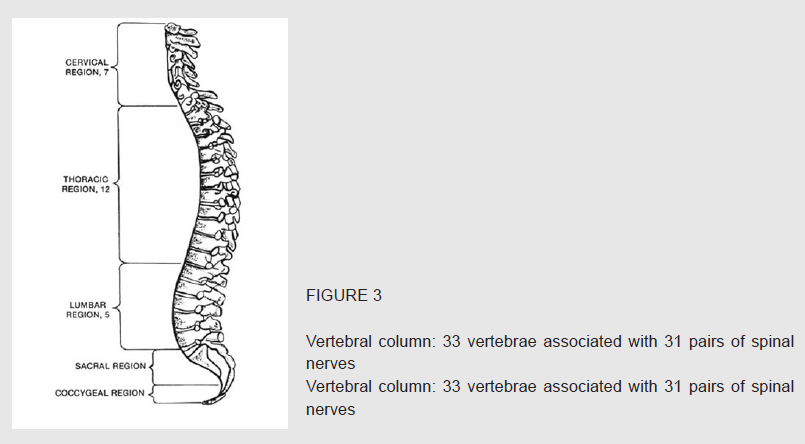
As the face and limbs form, the disks are stretched downwards and outwards. However, the sequence of the dermatomes remains unchanged even though they no longer look like a stack of coins. In the fully formed fetus there are 33 divisions in the spinal column. Each has a corresponding vertebra or bone – 7 in the neck (cervical vertebrae); 12 in the rib-cage or thorax (thoracic vertebrae); 5 in the small of the back (lumbar vertebrae); 5 in the sacrum (sacral vertebrae) and 4 in the tail bone (coccyx).
Without getting into the numbering of the associated nerves, which differs somewhat from the vertebrae, the general picture is apparent and it is illustrated in Fig. 4. Notice how each of the disks in the embryo has now become a dermatome.

The reason for providing this background is that injuries to the spinal cord or spinal nerve roots affect the motor function and / or sensory function within the respective dermatomes. The difference is that an injury to the spinal cord also affects the subsequent dermatomes to some extent as the nerve filaments are interrupted on their journey from head to tail. A spinal nerve root injury only affects that specific dermatome.
Paraesthesias or weakness in the distribution of a dermatome indicates probable spinal cord or spinal nerve root involvement. Although this may be due to other causes, such as a prolapsed intervertebral disk (i.e., the cushion of fibrous cartilage between vertebrae), these manifestations require urgent medical assessment. If there is associated weakness, paralysis or loss of bowel or bladder control, it is a medical emergency.

Peripheral Nerves
Peripheral nerves are the continuation of the filaments (i.e., axons) in the spinal cord. They form the unbroken electrical links between the brain and the target organs or tissues they supply. The first section of these nerves, as they leave the spinal cord, are called spinal roots. In the sections of the spinal cord supplying the arm and the leg, the spinal roots mingle and merge to become a tangle of nerves called the brachial (i.e., arm), lumbar, and sacral plexus (i.e., network or webs) respectively.
See Fig 6. The tangles eventually separate out into a number of blended peripheral nerves to supply the skin of the upper and lower limbs respectively.

This is one of the main reasons why there is a significant difference in the way spinal cord or spinal root damage presents itself vs. nerve plexus and peripheral nerve injuries, and why this background information is important: It allows us to make the necessary distinctions. Unlike damage to the spinal cord, which follows the “stacked” dermatomal pattern of sensory loss, injuries to the brachial plexus or peripheral nerves are patchy in nature.
Fig 7 shows the important patches of skin supplied by these peripheral nerves.

If numbness or tingling is limited to a seemingly random patch of skin and does not affect the entire limb (i.e., it is not cortical / regional) or a circumscribed segment (i.e., it is not spinal / dermatomal), then it is probably due to a peripheral nerve or nerve plexus injury. Importantly, from a management point of view, any injury or illness causing loss of strength, weakness or loss of function is always to be considered a medical emergency. Similarly, all anesthesia in an area that lasts more than a minute of two (e.g., due to direct mechanical compression of a nerve due to position or compression by diving gear, etc.) is in need of immediate medical attention. It is only in the area of partial sensory changes – or paraesthesias – where we would like to assist divers in distinguishing trivial from more serious injuries.
 Fig 8a shows the contrast between spinal / dermatomal vs. peripheral nerve distribution to the skin. This allows for easier distinction between the areas of skin that would be affected by injuries to the spinal cord or peripheral nerves respectively. (Fig. 8b)
Fig 8a shows the contrast between spinal / dermatomal vs. peripheral nerve distribution to the skin. This allows for easier distinction between the areas of skin that would be affected by injuries to the spinal cord or peripheral nerves respectively. (Fig. 8b)
Common diving-related injuries
Now that the distinction between dermatomal and peripheral nerve-related paraesthesias has been made, we will show five common diving-related conditions that are frequently attributed to DCI but are almost invariably related to a compressive injury of a peripheral nerve (Fig.9):

Pressure on the upper parts of the brachial plexus present as numbness of the lower part of the forearm including the hand. This is common with heavy BC’s in slender individuals.

Tight fitting wetsuits or leaning on the elbow may compress the ulnar nerve in the region of the cubital tunnel (i.e., the funny bone) causing numbness of the lower palm of the hand. Note, unlike the brachial plexus injury this excludes the forearm and is limited to the hand only (Fig.10).

Median nerve compression may occur due to a tight fitting wetsuit cuff, gloves or holding onto the boat gunnels during launching (Fig.11).

Pressure on the sciatic nerve due to sitting on a hard surface may cause numbness in a large area of the back of the leg. Boat rides are notorious (Fig.12).

Obesity and compression by a weight belt can cause an impingement of the lateral femoral cutaneous nerve resulting in paraesthesias of the upper outer thigh (Fig.13).
Summary
The purpose of this article is only to separate out the tingles that are not bends. Any injury or illness causing loss of strength, weakness or loss of function, including bowel or bladder function, is always to be considered a medical emergency.
All anesthesia in an area that lasts more than a minute of two (e.g., due to direct mechanical compression of a nerve due to position or compression by diving gear, etc.) is in need of immediate medical attention.
Paraesthesia or tingling is the result of a partial interruption of sensory nerve conduction between the skin and the sensory cortex Both paraesthesia and anaesthesia may be the result of damage to the brain, spinal cord or nerves. Large areas of numbness – especially if a whole arm or leg is affected and there is associated weakness or paralysis – are very suspicious of brain involvement and constitute a medical emergency.
Paraesthesias or weakness in the distribution of a dermatome indicates probable spinal cord or spinal nerve root involvement. Although this may be due to other causes, such as a prolapsed intervertebral disk (i.e., the cushion of fibrous cartilage between vertebrae), these manifestations require urgent medical assessment.
If numbness or tingling is limited to a seemingly random patch of skin and does not affect the entire limb or a circumscribed segment, then it is probably due to a peripheral nerve or nerve plexus injury.
The most common of these are compression or minor injuries of: (1) lower brachial plexus; (2) ulnar nerve; (3) median nerve; (4) sciatic nerve and (5) lateral femoral cutaneous nerve.
Remember – when in any doubt – contact Divers Alert Network for assistance and advice.

